This article starts Part 1 of a new series telling you all you Kneed to Know about the current treatment options for knee osteoarthritis. If you have dull, achy pain in your knees, difficulty getting around due to knee pain, have been told you have bone-on-bone, or if your doctor has been encouraging you to get knee injections or even a knee replacement, then this series is for you! If you’re not sure exactly what “knee osteoarthritis” is, check out my overview post here. If you really want to dive deep into what causes knee osteoarthritis and joint breakdown, check out my 4-part series on why knees break-down over a lifetime here, here, here, and here. If you’re ready to start getting a handle on your knee health, then you’re in the right place!
In Part 1, we are going to start with my personal favorite approach: lifestyle and behavior change.
What does “lifestyle and behavior change” mean?
Nearly all professional organizations and scientific committees recommend lifestyle and behavior change as the first-line, gold standard approach for managing knee pain and dysfunction due to osteoarthritis.
Lifestyle and behavior change approaches for managing knee osteoarthritis encompass all the treatment approaches that you can do on your own and do not require any surgery or drugs. These include:
- Education
- Weight-loss
- Exercise
You’ve heard the term “save the best for last”, well I’m going to do the exact opposite today. Lifestyle and behavior approaches for managing knee osteoarthritis are by far my favorite approach for three reasons. First, they are safe. Engaging in pharmaceutical or surgical approaches for knee osteoarthritis management can offer great benefits, but any intervention which introduces drugs or puts you under the knife carries intrinsic risks which we would like to avoid if we can. Second, they are accessible. Anyone, when given access to the right information (i.e., this blog!), can effectively use lifestyle and behavior change approaches to greatly improve their knee pain and function while delaying the need for pharmaceutical and surgical interventions. Lastly, they are effective. Many view lifestyle and behavior management approaches as a temporary fix until they can get the “real” solutions for osteoarthritis, but what people don’t realize is that nearly all professional organizations and scientific committees recommend lifestyle and behavior change as the first-line, gold standard approach for managing knee pain and dysfunction due to osteoarthritis. Even our most advanced pharmaceutical and surgical approaches often fail to meet the results provided by well-designed lifestyle and behavior management solutions. If you’re struggling with knee osteoarthritis, this is definitely the place to start!
Education
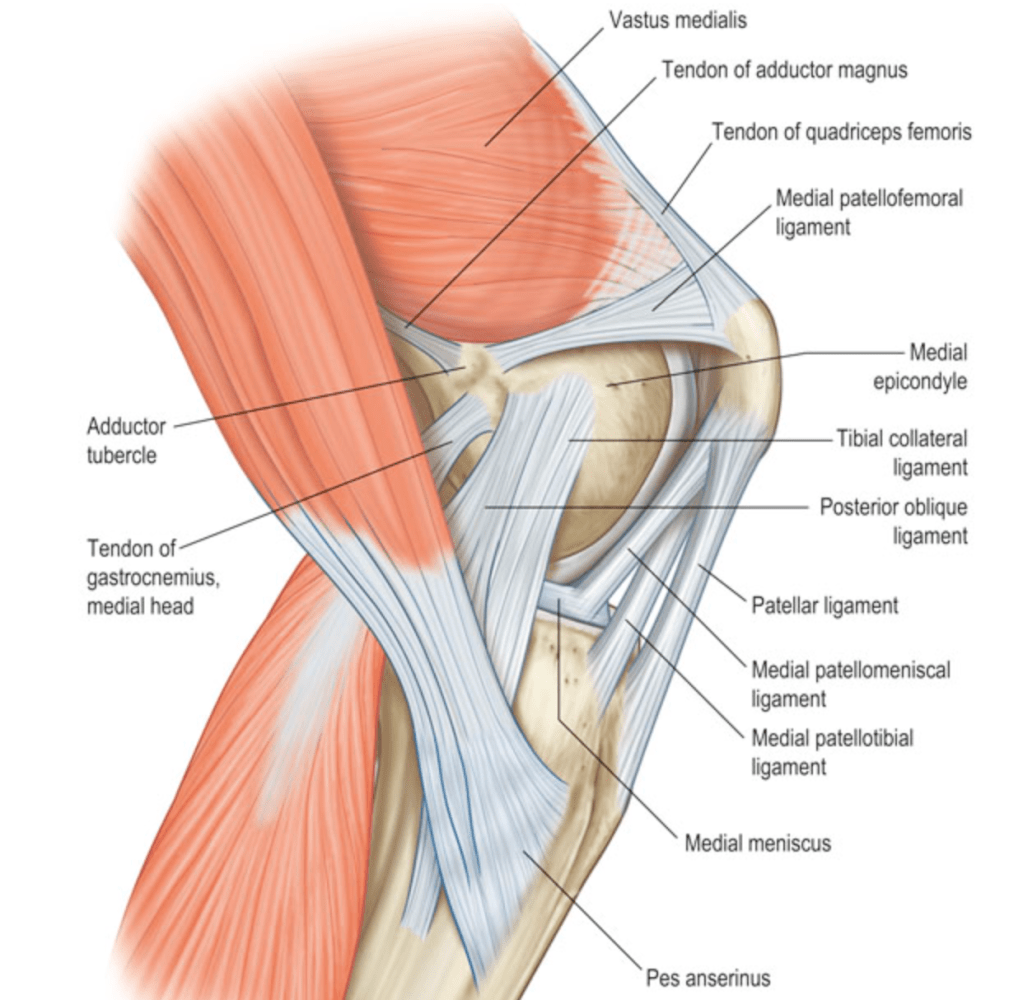
Getting to know what’s going on with your knees is the critical first step in managing knee osteoarthritis in a way that sticks. This includes: understanding the knee joint, what causes joint degeneration and pain, and how you can begin addressing disease progression and symptoms. Education takes you from a place of “My knee is stiff and painful and I don’t why!” to a place of “I know what is causing these symptoms and I have a plan for long-term health”. Simply demystifying the experience of your knee problems can work wonders for managing your own knee health. This is why scientific studies investigating simple education interventions focused on what happens during knee osteoarthritis and available treatment approaches are shown to be effective time-and-time again.
Granted, as you can imagine, scientific studies also repeatedly show that education + some sort of structured intervention protocol is almost always better than education alone. I add this section in here to say that simply becoming aware of the mechanisms of knee breakdown (like you are doing by reading this article) is a great first step on its own.
Weight-loss
I’ll preface this section by saying weight-loss is, of course, only effective for those who are already overweight or obese. If you do not fit this category, feel free to move straight to the next section. However, for those who are overweight or obese, weight-loss can be one of the most effective interventions for managing knee pain and symptoms related to knee osteoarthritis.
If you read my articles on how mechanical loading and inflammation contribute to knee breakdown, you already know how obesity can play a key role in the development and progression of knee osteoarthritis. Following sufficient weight-loss, people with knee osteoarthritis demonstrate faster walking speed, decreased compressive loading through the articular cartilage of their knee, and lower levels of inflammatory chemicals both in the whole body and in the knee joint. With these effects, it is no surprise that weight-loss has been shown to slow the progression of joint damage over time.
Even better, it does not take an extreme body transformation to see significant improvements in knee pain and function. Research has shown that just a 5-10% reduction in overall body weight can produce notable improvements in knee pain and function. With that said, there is a clear linear relationship between the amount of weight-loss and improvements in knee osteoarthritis. Stated simply, for as long as a person is over-weight or obese, the more weight they lose, the more improvements they will see with their knee pain.
There is one more important thing to consider before you go off on your weight-loss journey: muscle mass. We’ve already talked about the importance of muscle function for long-term knee health, but this gets highlighted again in the science of weight-loss for knee osteoarthritis. It has been shown that a loss of lean body mass (mostly muscle and bone) of greater than just 1% of your body weight can eliminate many of the positive effects of weight-loss for knee health. This is especially true for benefits pertaining to preservation of long-term function and mobility. When you put yourself in a calorie deficit to lose weight, you will lose fat (which is good if you are overweight or obese), but you also run the risk of losing muscle (which is not good). Thus, if you are starting a weight-loss journey to protect your knees, be sure to engage in frequent exercise and develop the right nutrition habits to preserve muscle mass while losing fat.
And this brings us nicely to the next section…
Exercise
Exercise is one of the most widely researched lifestyle and behavior change interventions for knee osteoarthritis. It continues to be validated time-and-time again to reduce pain, improve function, improve quality of life, and reduce the need for total knee replacement for people with knee osteoarthritis. This may sound simple enough; just exercise and your knees will get better! However, you may find yourself with questions like: what is exercise? and what is the best way to exercise for my knee health? Generally, exercise is a term which describes any intentional physical activity with the aim of improving your health, but this definition gives room for many different types of activities. To give some more specificity, I’ll talk about exercise in a few broad categories:
Aerobic exercise: Aerobic exercise is typically longer duration bouts of constant activity that elevates your heart rate and keeps it elevated for a period of time. We can further separate this category into low impact and high impact aerobic exercise. Low impact aerobic exercise includes activities such as cycling and walking. This type of exercise places minimal loads through your knees and, as such, has much lower risk for injury and joint irritation. Further, low impact continuous activity gives the articular cartilage of the knee a consistent flow of nutrients. For these reasons, a daily habit of low impact exercise can form a great base for any exercise program for knee osteoarthritis. This could be as simple as casually walking or cycling for 30-60 minutes every day. You may also engage in high impact aerobic exercise which includes activities such as jogging, running, and sports (tennis, basketball, etc.). These activities place higher amounts of loading and impact through your knees, so they bring the potential risk for joint injury and irritation. However, I certainly don’t say this to scare you away from engaging in these activities. Research has actually shown that lifelong runners may actually have a lower risk of knee osteoarthritis rather than the elevated risk that common knowledge might lead you to believe. All this to say that higher impact aerobic activities can be a safe and rewarding part of your knee health goals, but you must be a careful to progress into them the right way to avoid injury or damage (see more here).
Resistance training: Resistance training aims to directly improve the quality of your muscles by having them contract against external loads. This includes body weight exercises (such as push ups or lunges), free weight exercises (such as those which use barbells and dumbbells), and machine weight exercises (such as those which use weight-lifting machines commonly seen in gyms). Through resistance training you can increase your muscles’ ability to produce force (strength), their ability to produce force quickly (power), their ability to produce repeated contractions (endurance), and their overall size (hypertrophy). As I’ve talked about previously, these aspects of muscle function are absolutely critical for long-term knee health. In addition to improving muscle quality, resistance training can improve movement quality for those with knee osteoarthritis by helping them move faster, more efficiently, and with great shock-absorption. Moreover, resistance training can have a potent anti-inflammatory effect at the level of the knees and through the whole body through the release of anti-inflammatory myokines. Considering resistance exercise can regulate mechanical loading at the knee, attenuate inflammation, improve muscle quality, and optimize movement patterns, it is not a surprise that resistance training is one of the most supported and recommended interventions for those with knee osteoarthritis. A committed resistance training program has been shown to greatly reduce pain, reduce disability, and delay the need for total knee replacement amongst those with osteoarthritis. Similar to high impact aerobic training, I must again address the stigma that seems to pervade the public conversation around resistance training and knee breakdown. I have heard many patients say something like, “I have bad knees because I did too many squats in my 20’s”, but this sentiment is wholly unfounded in the vast amount of scientific literature on this topic. Maintaining muscle quality through resistance training actually reduces a persons risk of future knee degeneration, not the other way around.
Balance and coordination training: An often overlooked aspect of knee osteoarthritis is the loss of balance and coordination which comes with progressive joint degeneration. As the structures of the knee breakdown during the osteoarthritis process, the ligaments, tendons, nerves, and muscles which are responsible for communicating where your knee is in space and how it is moving begin to lose function. This is compounded by a general state of physical inactivity which further breaks down the position sense and coordination of the knee. When our brains do not get the correct information for where and how our knees are moving, it is very difficult to create coordinated and effective movement. This impaired coordination can lead to a greater risk of traumatic knee injury and a greater risk of trips and falls among those with knee osteoarthritis. Given the serious consequences of traumatic knee injury and falls, it becomes very important to maintain balance and coordination of the lower extremity as osteoarthritis progresses. This is where specific balance and coordination training comes in. This defines exercises which challenge your balance and coordination such as standing on one leg, standing on an uneven surface, or maintaining stability in complex environments (like sports activities). People with osteoarthritis show a great capacity to improve their balance and coordination through this type of training with improved mobility and a reduced risk of falls. Balance and coordination training alone has also been shown to improve the more traditional metrics of osteoarthritis like pain and function.
Aquatic Exercise: Lastly, I’ll give a nod specifically to aquatic exercise. This is a fancy term to describe any exercise which occurs in a pool or body of water. Aquatic exercise could easily be wrapped into any of the categories mentioned above depending on how you are performing the exercises in the pool, and, as such, they can confer just about any of the exercise benefits for knee osteoarthritis that I have previously mentioned. I’m giving aquatic exercise it’s very own section because 1) many people with osteoarthritis are specifically recommended aquatic exercise and 2) it does confer unique benefits that are not usually achieved in land-based exercise. Aquatic exercise has historically been advocated for as a specific remedy for knee osteoarthritis because the buoyancy of the water allows a person to perform exercise with reduced weight-bearing through the knee. Additionally, the pressure and heat of the water in many exercise pools can provide a pain relieving sensation to make exercise for those with knee osteoarthritis more comfortable. Despite this, most research shows a relatively equal effect of land-based and aquatic-based exercise for improving knee osteoarthritis outcomes. However, I am certainly not advocating that you discount aquatic exercise as an option. If you have access to a pool, and you find that being in a pool is a more comfortable and enjoyable way to perform exercise, then, by all means, take advantage of it!
With all these different types of exercise, I often get the questions “which is best? which one should I do?” However, these questions can be answered with a single blanket recommendation. All these types of exercises I have talked about have a great potential for benefit when done the right way and some potential for harm if done the wrong way, so there is not one style of exercise that is best in general terms. It all depends on what works for you based on your specific situation! When deciding which exercise approach works best for you, consider the following qualities of a good exercise program:
- Is the exercise accessible? You need to have the right resources to perform your chosen mode of exercise well. If you are interested in a type of exercise, but it is either not accessible or very difficult to access, then it is likely not for you.
- Is the exercise sustainable? A good exercise program should be something you can see yourself doing for an extended period of time. This means that the exercise is enjoyable (or at least enjoyable enough), not too expensive, and not too time-consuming.
- Does the exercise align with your goals? You want to make sure you choose exercise that is meaningful to you. If your goal is to be able to get up and down off the floor to play with your grandkids, then you should create an exercise program that will allow you to do that for a lifetime.
- Can you progress the exercise? The last key tenet of an effective exercise program is progressability. You should choose exercises, or an avenue of exercise, which you can make a little tougher each time you do it. Constantly meeting new exercise demands is the best way to continually make progress and ensure long-term knee health.
With all of that said, here’s a general structure for piecing together an exercise program:
- Every day, you should perform at least 30 minutes of low-impact physical activity such as casual walking, cycling, golf, or anything else in this category you may find enjoyable. This does not need to be, and shouldn’t be, very rigorous. Just something to keep your knees moving and lubricated.
- Once or twice a week, you should perform resistance training for all the key muscle groups of the lower extremity (more details here). This could be as simple as using the circuit of machine weights at your local gym, or as complex as power-lifting or cross-training with free-weights (assuming you have the right experience and coaching).
- Once or twice a week, you should incorporate some form of balance and coordination exercise. This could be in the form of single leg resistance training, simple balance exercises (like standing on one leg or an uneven surface), or structured balance and stability work like Yoga, Tai chi, or Pilates.
- Lastly, you may choose to engage in higher impact aerobic or sports activities such as running, basketball, or tennis. Including these activities in your exercise program is entirely based on your goals and preferences. It is a great thing to engage in communities centered around physical activity, so I would highly encourage you to explore them. If you choose to participate in some of these higher impact activities, be sure to progress into them slowly, listen to your body and potential knee pain, and prepare your body for these strenuous activities through the exercises outlined above.
Resources for getting started
Admittedly, lifestyle and behavior change can be one of the more challenging treatment approaches for knee osteoarthritis simply because it asks that you take responsibility for your knee health into your own hands. Weight-loss and exercise ask more of you than simply having a physician give you a pill or injection. But trust me, you will not regret it once you start building these habits. So how can you get started?
Education: This is a simple one because you are already doing it! After reading this article, remain intellectually curious about you knee health and pay attention to how your knees respond to different movements, activities, and interventions. The more in-tune and knowledgable you are about your knee health, the better equipped you will be to address it.
Weight-loss: First, I would encourage you to consult your primary care physician before starting a weight-loss program. Assuming you are clear to start losing weight, the best option would be to hire a coach, nutritionist, or dietician to design a weight-loss plan for you. This can take the vast majority of the complexity out of the process. If hiring an expert is not an option for you, you can stick with the tried-and-true “calories in, calories out” approach. While it is far from a perfect model for health, you will lose weight if you consume less calories than you burn. A resource like this can help you determine your caloric needs and give you a baseline for your weight-loss plan. Without going into too many specifics, I would also recommend that you consume sufficient protein to avoid losing muscle during this process. At least 0.7 grams of protein per pound of body weight would be a good target, but up to 1.0 gram of protein per pound could help ensure maintenance of muscle mass especially if you are performing resistance training as recommended above.
Exercise: Beyond following the guidelines I listed in the exercise section, I would encourage you to get acquainted with the resources you have available to you. Many local community centers have free or low-cost access to exercise programs for a wide range of ages and physical activity levels. Some areas even have specific programs for knee osteoarthritis. You can also look into community groups in your area. These could be self-organized groups of people who walk together, do yoga together, or even jog together. If you’re in generally good health, and just want to build a habit of exercise, the best option would be to hire a certified personal trainer or coach to at least show you the ropes and get you started. If you’re already having knee pain which is limiting you from certain activities, or if you have other impairments or diseases which make exercise difficult, I would highly encourage you to work with a physical therapist to design an exercise program to get you out of pain and keep you moving well for a lifetime.
With all of that said, I do have to give one last shameless plug for my own content. I have written a book, Health Simplified, which gives a step-by-step approach to incorporate healthy habits into your lifestyle. While it is not specifically focused on knee osteoarthritis, it gives a lot of great information and tips related to the things I have talked about in this article.
While I firmly believe in lifestyle and behavior approaches for managing knee osteoarthritis, you will inevitably encounter many other treatment options on your knee health journey. Join me in Part 2 of this series as I talk all about pharmaceutical management of knee OA!





Leave a comment