Welcome back to my series on why knees break down over a lifetime! In Part 1, we covered how the mechanical loads placed through the knee joint contribute to knee breakdown and how they can also contribute to preserving knee health. Specifically, we discussed how mechanical loading placed through the knees must remain in the “goldilocks zone”, where loading is neither too much nor too little, if we want to keep the padding in our knee joint (the articular cartilage) healthy for the long term.
In Part 2 of this series, we will discuss the second big contributor to knee breakdown: Inflammation.
So what is inflammation?
To be honest, inflammation gets a bad rap. Whenever you hear anyone talking about inflammation, it’s usually about preventing or reducing inflammation. However, inflammation is actually the critical first step in the body’s healing process. When your body senses damage or injury, the inflammatory process begins to do the following:
Increase blood flow: Blood flow is critical for the healing of nearly all body tissues. Blood provides our tissues with oxygen and nutrients that are critical for the repair of damage. Further, increased blood-flow facilitates the recruitment of other healing factors (talked about next) to the area. This increase in blood-flow is what causes the redness, heat, and swelling that we often associate with inflammation.
Recruit immune cells to the area: Another important function of inflammation is to recruit immune cells to the area of damage. These immune cells need to be available to address any viruses, bacteria, or other foreign materials which could have entered the body at the time of injury.
Recruit enzymes and growth factors to the area: In order to begin healing from an injury, the body must first break down the damaged parts of the tissue, then it must begin to build up new tissue. This is initiated by first recruiting enzymes to break down and recycle damaged tissue components, and then growth factors are brought in to stimulate the rebuilding of that tissue. In a healthy immune response, there is a careful and well-executed balance of tissue breakdown and rebuilding which facilitates proper healing after injury.
Increase local sensitivity to pain: While this may seem like a bad thing at first, it can actually be quite beneficial. If a tissue in your body is injured, it is likely best to avoid stressing that injured tissue for at least a little while. This is where pain comes in. The temporary increase in pain caused by inflammation is your body’s way of telling you “take it easy for a bit”.
How does inflammation contribute to knee breakdown?
If inflammation is a healthy and beneficial part of the healing process, how does it cause knee breakdown? Well, inflammation is only healthy and beneficial when it lasts for a short period of time after an injury or tissue damage. In healthy knees, it is normal and expected to see a short-lived inflammatory response in the knees after high intensity activities. You work your knees hard, the inflammatory process rushes in to promote healing and repair of the tissues in your knees, and the inflammation is cleared out in a few hours. It is even normal to see inflammation in response to minor or moderate knee injuries. You may tweak your knee during activity, and afterwards your knee is a little swollen, hot, and painful, but with ice, rest, and active recovery, you are back to normal in a few weeks.
Inflammation really starts to become a problem and contribute to knee breakdown when it becomes excessive and prolonged. Like I said, inflammation is only supposed to be around for a few hours to a few days, but when it begins to hang around for weeks, months, or even years, inflammation starts to become a bad house-guest…
With prolonged inflammation in the knees, the enzymes and growth factors which once maintained a careful balance of breakdown and growth to maintain tissue health begin to transition more and more into tissue breakdown. These enzymes begin to attack the building blocks of the articular cartilage causing it to wear down over time, and the growth factors begin to promote the growth of bone spurs (called osteophytes) around the edge of the knee joint. Even worse, as the cartilage breaks down, the cells in the cartilage begin to release inflammatory chemicals in response to the injury.
Those immune cells which were once standing guard for any bad actors entering the body begin to linger and recruit their friends. Eventually, more and more immune cells build up in the knee, specifically, they tend to build up in the outside capsule or lining of knee joint (leading to something called synovitis). From here they actually begin to create more inflammation by the release of inflammatory chemicals. This further exacerbates and prolongs the already problematic inflammatory environment of the joint.
The heightened pain response which was originally designed as a helpful reminder to “take it easy for a while” now becomes a prolonged hinderance to daily activities. Pain in the knees from inflammation and tissue damage begins to make it difficult to participate in exercise, recreational, or even just daily life activities. This pain encourages a lack of physical activity and movement which leads to sedentary behavior and ultimately greater stiffness, pain, and degeneration in the knees.
Lastly, prolonged inflammation in the knee joint has an effect to make that “goldilocks zone” of the articular cartilage more and more narrow. Inflammation makes the articular cartilage more sensitive to mechanical loading, so that loading which was once beneficial to the cartilage becomes damaging. Thus, it becomes harder and harder to recover joint health as inflammation and damage progresses.
What causes prolonged inflammation in the knees?
Poor mechanical loading: As we’ve discussed in Part 1, mechanical loading plays a key role in knee breakdown, and one of the big reasons why mechanical loading is so important is inflammation. Very high loads through the articular cartilage and other joint tissues can cause these tissues to release inflammatory chemicals into the knee joint. Remember, this can be a normal thing if it happens every now-and-then and if your body recovers quickly, but this can become a problem if your knees are exposed to excessive loads ALL the time (in cases such as poor movement patterns, excessive exercise participation, obesity, etc.) creating a chronic inflammatory response. Interestingly, persistent decreased loading of your knees can also lead to a chronic inflammatory response. This further highlights the importance of exercising the right amounts and in the right ways.
Obesity: Excessive fat on the body is also a very common contributor to chronic knee inflammation and eventual knee breakdown. We’ve already discussed one reason why this is the case, and this is due to the added body weight dramatically increasing the loads through the knee with every movement. This makes a person who is obese more prone to excessively loading the knee tissues. Beyond the effect of added body weight, fat tissue also releases pro-inflammatory chemicals which contribute to a low-grade inflammatory response throughout the body. When fat mass becomes very high (as is the case with obesity) this whole-body inflammation can begin to affect the joints and contribute to breakdown.
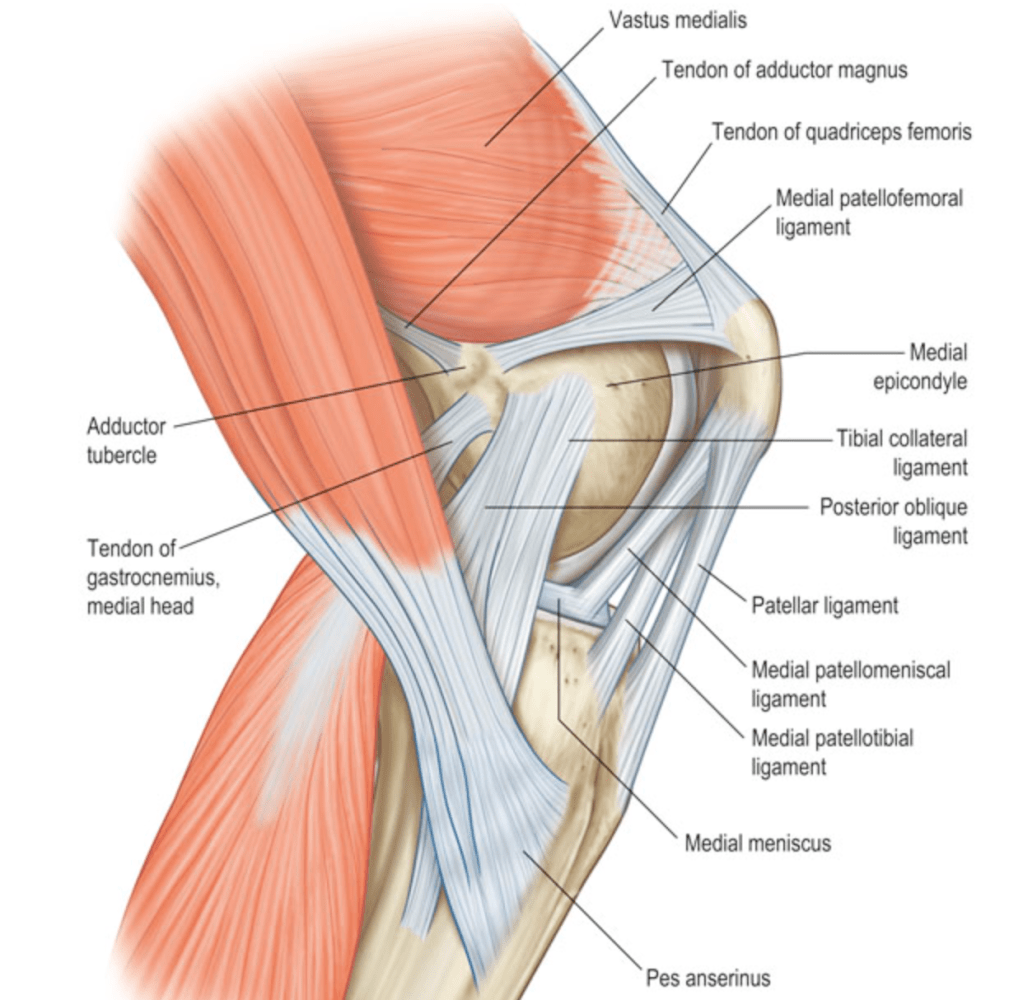
Traumatic knee injury: Breaks or tears to the bones, ligaments, tendons, and cartilage of the knee joint are very common cause of persistent inflammation in the knees. When a traumatic knee injury creates a massive disruption in the integrity of the knee joint structure, it is very likely that we will see an inflammatory response that lasts months or even years after the initial injury. For this reason, it is very important to rehab the right way after knee injury to mitigate the damaging effects of this prolonged inflammation
Arthritis: At first glance, this may seem confusing. We’ve talked about how inflammation causes knee breakdown associated with arthritis, not the other way around, right? Well that’s the tricky thing about osteoarthritis; it starts a vicious cycle where inflammation and joint damage actually creates more inflammation and joint damage. Joint tissues affected by arthritis begin to chronically release pro-inflammatory chemicals. Also, there are other forms or arthritis, such as rheumatoid or psoriatic arthritis, that can initiate massive inflammatory responses in the knees to induce joint breakdown.
What can we do about inflamed knees?
There are many ways that we can mitigate the damaging effects of knee inflammation. We may address it through lifestyle and behavior modifications, such as weight-loss, exercise, ice, and changing activity level. We also commonly address knee inflammation through anti-inflammatory medications, like over-the-counter non-steroidal anti-inflammatory drugs (ibuprofen/Advil) or steroid injections provided by your doctor. Lastly, you may have heard of more experimental methods of addressing knee inflammation like stem cell injections and platelet-rich plasma (PRP).
With all of these options, it can be daunting to chose an approach to manage knee inflammation. If you are wondering which option to take, ask your doctor or physical therapist about which one may be right for you. Also, you can check out my series on managing osteoarthritis (upcoming) to learn more about each of these options!





Leave a comment